Retinal detachment is when the retina separates from the back of your eye.
The role of the retina is to send signals to your brain when light enters your eye, which then gets interpreted as the images you see. However, If the retina detaches and isn’t in the right position, your vision can become increasingly distorted and blurred.
Retinal detachment usually just affects one eye but can affect both and are most common in people aged between 60 and 70.
Types of retinal detachment
Rhegmatogenous retinal detachment
This type of retinal detachment happens if a tear or hole develops in your retina which causes fluid in your eye to seep underneath your retina and therefore separate it from the back wall of your eye. This is the most common type of retinal detachment.
Tractional retinal detachment
In this type of retinal detachment, your retina is pulled away by scar tissue within your eye which can be caused by an abnormal growth of blood vessels in your eye, commonly found in people with diabetes. However, it can also occur if you injure your eye or have inflammation within it.
Exudative retinal detachment
This occurs when the blood vessels underneath your retina start to leak fluid and builds up underneath your retina. This can sometimes cause your retina to detach. This is quite rare.
Symptoms of retinal detachment 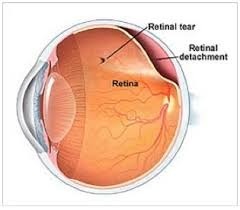
Retinal detachment is not painful, but you can often get warning signs beforehand such as blurred vision, the sudden appearance of floaters or flashes of light.
You may also experience a shadow spreading across the vision of one eye and your sight may be severely affected.
Treatments for retinal detachment
Retinal detachment can be treated by surgery to reattach the retina. There are different treatments available depending on the type of retinal detachment and how much of your retina has become detached. Luckily in more than 80% of cases, only one surgical procedure is needed to treat the detachment.
If the retina is not fully detached then there is the option of the following treatments to repair any tears or holes
• Laser surgery (photocoagulation). The surgeon directs a laser beam into the eye through the pupil. The laser makes burns around the retinal tear, creating scarring that usually “welds” the retina to underlying tissue.
• Freezing (cryopexy). After giving you a local anaesthetic to numb your eye, the surgeon applies a freezing probe to the outer surface of the eye directly over the tear. The freezing causes a scar that helps secure the retina to the eye wall.
If the retina is fully detached then one of the following treatments may be carried out depending on the type of detachment
1. Pneumatic retinopexy – This is a procedure that involves your doctor injecting a small gas bubble over the site of your detachment, without removing any of the vitreous. This then presses the retina back in place.
2. Scleral buckle surgery – This is when your doctor attaches a thin band of synthetic material to the outside of your eye. This presses on the outside of your eye causing the inside wall of your eye to move inwards slightly and push inside of your eye against the detached retina to help it re-attach.
3. Vitrectomy – This is when your doctor removes the vitreous (clear gel) from the back of your eye and replaces it with a silicone oil bubble which holds your retina in place while it heals.
Recovery after your operation will depend on the nature of the detachment and the treatment you received. After surgery you will be given some eye drops to prevent any infection and reduce swelling. Your vision should start to improve over the following days, but it can take a number of weeks.
If you have surgery using a gas or oil bubble you may be asked to posture after your operation for up to 10 days. This means that you will be asked to keep your head in a certain position to allow the gas or oil bubble to float into the best position to support the retina.
Whatever your treatment your ophthalmic surgeon will discuss your post-operative care and any concerns you may have such as when you can return to driving.
“I had cataract operations on both eyes in 2018 and my eyesight was good. In December 2019 I hit my head on a cooker extractor and felt dazed but recovered quickly.
The next day I noticed a vertical line which was black on one side in my right eye. I called into my favourite optometrist in Burnham who diagnosed a detached retina, and this was confirmed by the emergency department at Windsor.
The next day I had the retina reattached at the John Radcliffe hospital in Oxford. I had to ‘position’ for a week and after eight weeks my eyesight had returned.
In July I noticed a patch spreading across my left eye – much the same as a bleed and had the same operation at Reading. This time the recovery was much quicker; the gas bubble disappeared in only two weeks although my sight is only at about 75% of its previous capability.”
Mike Goodchild
Early action improves results
Retinal detachment can cause permanent loss of vision so it’s vital that you seek expert advice as soon as you experience any symptoms. If detected and treated early your vision may not be adversely affected. If you have any concerns please call us on immediately on 01628 663055
More information and support
Download – Understanding Retinal Detachment
RNIB Sight Loss Helpline 0303 123 9999